Syncope Rules?
We all love syncope with its ubiquity and complexity. Most causes are benign but the needle in the haystack may be
fatal. Wouldn’t it be nice to have a good clinical decision instrument to help us out?
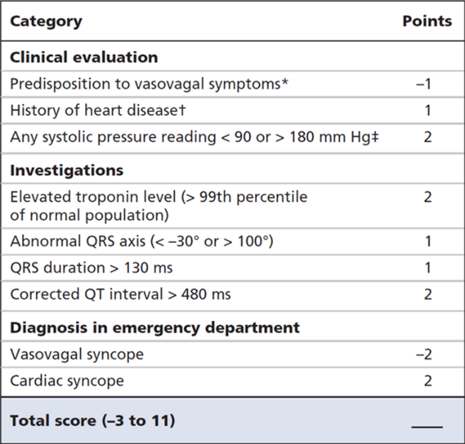
These researchers sought to validate the Canadian Syncope
Risk Score (see below) among 3819 patients that presented across 9 ED’s in Canada.
The risk score is mostly a quantification of what we evaluate
already. History, ECG, ED diagnosis and troponin (if performed). Score ranges
from -3 to 11 and patients are put into one of five categories; very low, low,
medium, high or very high risk.
The primary outcome was “30-day serious outcomes” as
determined during medical record review, telephone follow up, return visits, and
coroners’ database.
Results?
The proportion of patients with serious outcomes increased from
0.3% in the very low risk group to 51% in the very high risk group.
This seems ok but I’m not so sure this “rule” will gain
traction.
First, it’s too complicated to commit to memory. We would need
to refer to MDCalc which will decrease its utility.
Second, it hasn’t formally been compared to what we already
do… which is gestalt. (However, some may argue that it is already heavily
reliant on gestalt.) It is possible that following the rule could make things worse.
Third, we know rules tend to perform less well in complex
disease processes. This is why doctors have not been replaced by robots… yet.
How might I use the rule?
Probably how we use most rules; something we can write in
the medical record to support a decision we have already made. This might sound
cynical, but gestalt is probably the best rule.
Covering:
Thiruganasambandamoorthy V, Sivilotti M, Le Sage N, et al.
Multicenter Emergency Department Validation of the Canadian Syncope Risk Score.
JAMA Intern Med. 2020;180:737-44. [link to article]
No comments:
Post a Comment