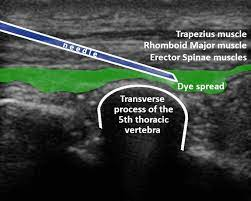
This study out of UC San Diego set out to determine the accuracy of lung ultrasound vs. supine portable chest x-ray for the detection of traumatic pneumothorax.
Yes, I also
thought this research questions had been suitably answered.
In 2020, a CochraneReview included 13 prospective paired comparative accuracy studies and
concluded that ultrasound was about 90% sensitive vs. 50% for a chest x-ray. Both
are highly specific.
Regardless
of the consistent evidence, let’s consider face validity. Anyone who is
competent in lung ultrasound knows that ultrasound is much better at finding
pneumothorax. There is no planet in the solar system where a supine portable
chest x-ray is going to be more sensitive than ultrasound.
But this study concludes the opposite… chest x-ray was better!
Huh? How could this be?
This was a
retrospective registry review. Retrospective data is often poor quality. Registry
data is even worse. Garbage in... garbage out. Ironically, this study would never have been included in
the Cochrane review.
What is the
probability that this single study with worse quality evidence is correct and all
the consistent higher quality studies are wrong?
Yes, the
probability is close to zero.
But where
did this study really go wrong?
I think the
authors answered the question themselves, “… in a non-study environment,
such as ours, the pleural views were not universally performed with the same
rigor as in a prospective study designed specifically to detect pneumothorax.”
I think
this is probably the answer.
There are many other problems with this study, but I’m limited by word count. So briefly, the methods for assessment of diagnostic accuracy of a test were performed backwards. They used the wrong probes for lung ultrasound. They used the wrong clinicians to perform and interpret the ultrasound. That was only to name a few...
As expected,
there were many concerned letters to the editor. Even one from Dr Giovanni Volpicelli who
is the world leader and pioneer of lung ultrasound. But the authors stuck with
the strategy of “never admit you are wrong” and doubled-down in their conclusions.
A bit sad really...
Covering:
Santorelli JE, Chau H, Godat L, et al. Not so FAST- Chest ultrasound underdiagnoses traumatic pneumothorax. J Trauma Acute Care Surg.2022;92:44-8.[link to article]